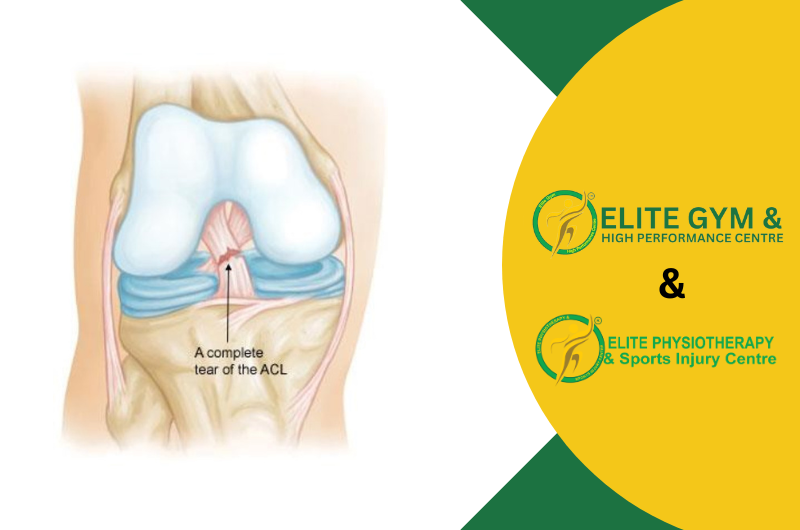
What is the Cross Bracing Protocol?
For certain acute ACL ruptures, the Cross Bracing Protocol (CBP) is a time-sensitive, non-surgical treatment option. For the first four weeks, the knee is in a 90° flexion position. After that, the brace is gradually unlocked to restore motion, to mimic the remaining ACL so that the native ligament can repair. Early results from prospective cohorts report high rates of MRI continuity at 3 months; clinical trials are still being conducted to determine suitable individuals and longer-term outcomes.
Why it matters
A totally ruptured ACL was formerly thought to be incapable of healing, necessitating early repair or conventional rehabilitation without bracing. Recent data casts doubt on that belief. In a secondary analysis of the KANON trial, approximately one-third of ACLs treated solely with rehabilitation had MRI evidence of healing at two years (and roughly one-half when those who underwent surgery were excluded), and the healed group had better patient-reported outcomes. By purposefully placing the knee to encourage tissue apposition as soon as possible after injury, CBP enhances this healing potential.
Who is (and isn’t) a Candidate?
The best candidates typically show up early (preferably within 10 days after the injury), have an MRI showing an acute ACL rupture, and can follow bracing and follow-up instructions to the letter. MRI morphology (such as remnant quality, displacement, and gap distance) and patient characteristics (sport demands, support, and comorbidities) are progressively taken into account during the selection process.
Not suitable for all: Clinicians are frequently pushed onto alternative approaches due to multi-ligament injuries, displaced bucket-handle meniscal tears/loose bodies requiring urgent surgery, extremely delayed presentation, or enhanced thrombosis risk. (CBP-using programs typically sort them out in the early stages of MRI-guided decision making.)
How the Protocol Works
The basic idea is to protect the healing ACL from anterior tibial translation and pivoting by initially reducing and immobilizing (similar to a fracture) and then gradually restoring motion every week.
Weeks 1–4
- Brace: locked at 90° (24/7; sleep in brace).
- Weight-bearing: Non-weight-bearing (NWB) with crutches.
- Goals: protect the healing zone, maintain patellofemoral mobility, prevent deconditioning (safe isometrics).
5th Week
- Brace 60–90°. Continue NWB. Begin gentle, brace-permitted ROM drills; progress isometric hamstring/quadriceps sets in allowed angles.
6th Week
- Brace ~45–90°. Still NWB. Add stationary bike within brace limits if permitted.
7th Week
- Brace 30–120°. Partial weight-bearing begins; gait retraining within brace range. Light closed-chain work in safe angles.
Week 8
- Brace 20–120°. Progress PWB loading, proprioception in brace.
Week 9
- Brace 10–120°. Full weight-bearing as tolerated in brace; advance strength, balance, conditioning tasks (pool if available) without pivoting/cutting.
Weeks 10–11
- Unrestricted brace during the day; remove for sleep. Continue progressive strengthening, linear conditioning, and landing mechanics in straight plane.
Week 12
- MRI and clinical review. The brace is taken off, and criterion-based rehabilitation continues if the MRI reveals sufficient continuity and clinical stability. If not, a “cross-over” to surgery or an extension of bracing may be part of the collaborative decision-making process.
Beyond 12 weeks (typical milestones)
- Weeks 16–17: Start straight-line running (criteria-based).
- ~6–12 months: Athletes gradually return to training and then progress to sport-specific change of direction once they achieve goals for strength, symmetry, hop testing, and movement quality. Many programs plan for nine to twelve months before a complete return to pivoting sports.
Rehabilitation Priorities
Protection & monitoring (0–12 wks)
- Teach people to use crutches, wear braces strictly, and refrain from twisting or pivoting.
- Ankle pumps, hip/glute/hamstring isometrics, and early patellar mobilization (knee maintained within brace limits).
- Some programs aggressively monitor DVT risk (local techniques vary; some reported early DVTs spurred teams to embrace pharmacologic prophylaxis).
Strength & motor control (weeks 5–12)
- Avoid anterior shear (no open-chain knee extension in vulnerable ranges) and increase closed-chain strength in safe arcs.
- Brace ROM connects directly with balance, trunk/hip control, and graded conditioning (bike, pool, and later treadmill).
Run-jump-cut reconditioning (post-brace)
- Linear running → decel/accel → low-level plyometrics → planned change-of-direction → unplanned COD and sport skills after meeting patient-reported outcomes targets and ROM/strength/hop/movement benchmarks.
To prevent vasoconstriction during the initial healing window, some CBP teams prohibit the use of NSAIDs, knee aspiration, and even cryotherapy.
What Does the Evidence Say (so far)?
- High MRI early healing with CBP: Three months after CBP, a prospective cohort reported ~90% ACL continuity, and patients with greater early MRI healing achieved better results. Researchers still need randomized longer-term results.
- In certain situations, ACLs can heal without surgery: In the KANON dataset, MRI showed healing in around 30 to 50% of patients who underwent rehabilitation alone, independent of CBP.. The KOOS results of the healed groups were better than those of the non-healed/reconstructed groups.
- Risk-benefit balance: Although reviews point to encouraging healing, they also emphasize the danger of stiffness, the necessity of careful selection and adherence, and the possibility that some patients will require surgery.
CBP vs. Traditional ACL Management
| Dimension | Cross Bracing Protocol | Traditional Reconstruction / Standard Non-Op |
| Primary goal | Heal the native ACL (biologic healing) | Replace with graft (surgery) or compensate via neuromuscular rehab |
| Early positioning | Immobilize at 90° flexion for 4 weeks, then staged ROM | Prioritize full extension early; brace often locked in extension initially post-op; no prolonged flexion immobilization |
| Weight-bearing (early) | NWB first weeks; add load as brace range increases | WBAT early after ACLR; progress as swelling/quad control allow |
| ROM strategy | Delayed extension; weekly unlock schedule | Immediate mobilization, especially regain full extension to avoid arthrofibrosis |
| Cryotherapy & NSAIDs | Some programs limit early NSAIDs/icing (program-specific) | Commonly used to control pain/effusion post-injury/surgery |
| Monitoring | Scheduled MRI at ~3 months to confirm continuity | Imaging usually not required once post-op course is stable |
| Time to pivot sports | Typically ≥9–12 months and criteria-based | Also ≥9–12 months and criteria-based (graft maturity & testing) |
| Key risks | Stiffness/extension loss if mishandled; non-healing → cross-over to surgery | Graft failure, donor-site morbidity, cyclops lesions, and surgical risks |
| Time to pivot sports | Motivated, early-presenting patients willing to adhere strictly; favorable MRI pattern | Graft failure, donor-site morbidity, cyclops lesions, surgical risks |
At Elite Physiotherapy and Sports Injury Centre, we integrate the latest evidence-based approaches, such as the Cross-Bracing Protocol (CBP), alongside traditional ACL rehabilitation and surgical recovery programs. With our advanced facilities—including Super Inductive Stimulation (SIS), Class 4 Laser Therapy, CRET Therapy, Shockwave Therapy, and Hydrotherapy—we ensure that every patient receives a personalized, high-end rehabilitation plan. Our focus is not just on healing the ligament but also on restoring strength, balance, and performance, so athletes and active individuals can safely return to their sport or lifestyle with confidence.