Understanding the Radial Collateral Ligament of the Elbow
- An important factor in joint stability is the elbow’s Radial collateral ligament.
- It shields the elbow from undue varus strain.
- Additionally, it keeps the forearm rotating smoothly during everyday and athletic tasks.
- We regularly treat Radial elbow instability in athletes and active people at Elite Physiotherapy and Sports Injury Centre.
What Is the Radial Collateral Ligament of the Elbow?
- The Radial collateral ligament complex lies on the outer side of the elbow.
- It joins the ulna to the Radial epicondyle of the humerus.
- It provides both static and dynamic stability by collaborating with the surrounding muscles.
- During pushing and weight-bearing activities, it stops the elbow from opening abnormally.
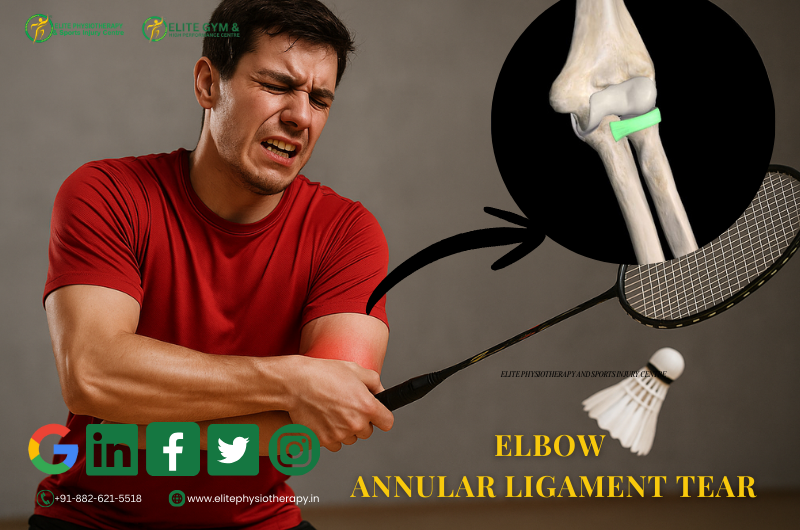
Components and Classification
- The Radial collateral ligament is a complex structure.
- It includes several distinct parts.
- Radial Collateral Ligament
- Lateral Ulnar Collateral Ligament
- Annular Ligament
Causes of Radial Collateral Ligament Injury
- Overload or trauma are the most common causes of Radial ligament injury.
- The following are typical causes.
- Fall on an outstretched hand with elbow extension
- Repetitive pushing activities
- Throwing sports with poor biomechanics
- Elbow dislocations
- Sudden varus stress during contact sports
- At Elite Physiotherapy, we also see chronic injuries from improper training load.
Clinical Features and Symptoms
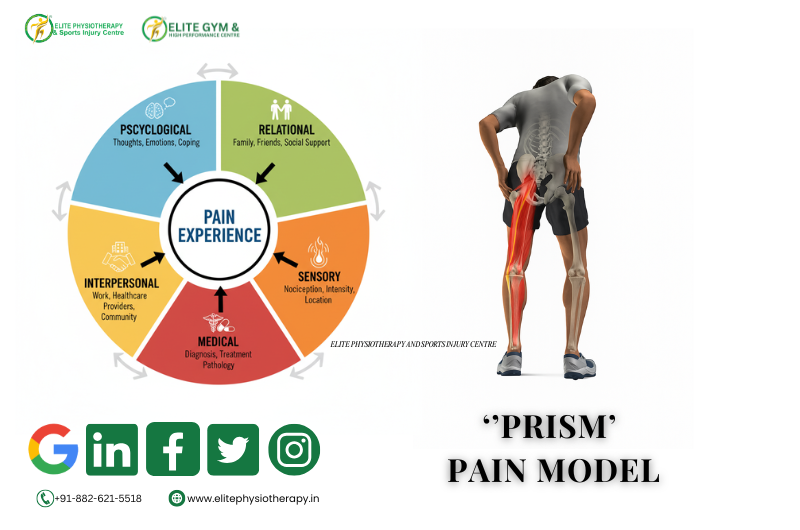
- The intensity of the injury determines the symptoms.
- Nonetheless, the following are typical clinical characteristics.
- Pain in the lateral elbow
- A sense of weakness or instability
- Pain when pushing out of a chair
- The sense of clicking or catching
- Inadequate grasp strength
- A decrease in self-assurance when participating in sports
- When bearing weight on the hand, pain often worsens.
Diagnostic Methods and Investigations
- Accurate diagnosis is essential for complete recovery.
- At Elite Physiotherapy and Sports Injury Centre, we follow a structured approach.
- Clinical Examination – Detailed history, Palpation, Range of motion, and functional tasks are assessed carefully.
- Imaging Investigations- MRI provides a detailed visualization of ligament damage.
Physiotherapy Assessment Techniques
- Varus Stress Test
- Posterolateral Rotatory Instability Test
- Chair Push-Up Test
Physiotherapy Management at Elite Physiotherapy and Sports Injury Centre
- Physiotherapy is the first line of treatment in most cases.
- Our management is individualized and sports-specific.
Phase 1: Pain and Protection
- Initially, the focus is on pain control.
- Activity modification prevents further ligament stress.
- Cryotherapy and protective taping are used strategically.
- Early gentle mobility prevents stiffness.
2nd Phase: Restore Mobility and Muscle Activation
- Gradual range of motion exercises are introduced.
- Forearm, wrist, and elbow mobility are restored carefully.
- Isometric strengthening begins for pain-free activation.
- Scapular stabilizers are trained simultaneously.
3rd Phase: Strengthening and Dynamic Stability
- Progressive resistance exercises are introduced gradually.
- Emphasis is placed on the wrist extensors and flexors.
- The flexor-pronator and extensor-supinator groups are strengthened.
- Closed-chain exercises improve joint co-contraction.
- Proprioceptive drills enhance neuromuscular control.
Phase 4: Functional and Sports-Specific Training
- Functional loading prepares the elbow for real demands.
- Physiotherapists retrain throwing, pushing, or grappling patterns.
- Kinetic chain integration reduces elbow overload.
- Clinicians follow return-to-sport criteria strictly.
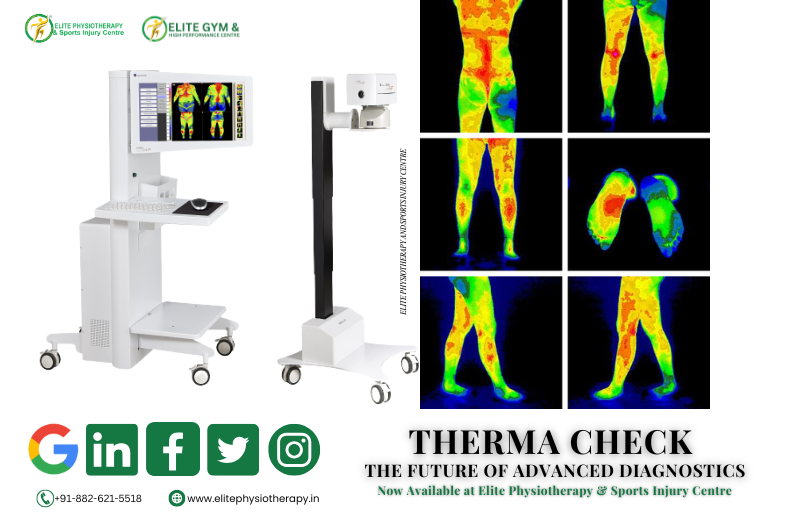
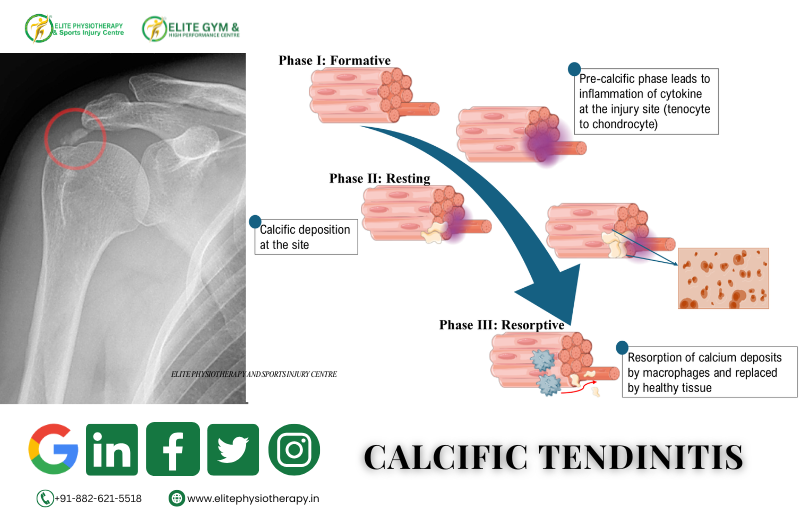
Advanced Physiotherapy Modalities Used
- At Elite Physiotherapy, advanced technology enhances recovery.
- Shock Wave Therapy
- Super Inductive System
- High Intensity Laser Therapy
- Dry Needling and Cupping Therapy
Prevention and Long-Term Care
- Prevention is essential for lasting elbow health.
- Correct biomechanics reduce ligament stress.
- Strength balance across the upper limb is crucial.
- Regular mobility and recovery sessions prevent overload.
- At Elite Physiotherapy, education is part of every program.
Why Choose Elite Physiotherapy and Sports Injury Centre?
- We combine clinical expertise with advanced technology.
- Physiotherapists personalize every program and focus it on clear goals.
- Athletes receive sport-specific rehabilitation strategies.
- Our focus remains on safe return to performance.
Final Words
- You should never ignore Radial collateral ligament injuries.
- Early physiotherapy ensures stability and confidence.
- With expert care, full recovery is achievable.
Book your assessment at Elite Physiotherapy and Sports Injury Centre today.