Introduction
Shoulder dislocation is a prevalent injury, especially among athletes and active individuals. Our specialty at Elite Physiotherapy & Sports Injury Centre is offering cutting-edge, individualized treatment to promote the best possible recovery and avoid recurrence.
Understanding Shoulder Dislocation
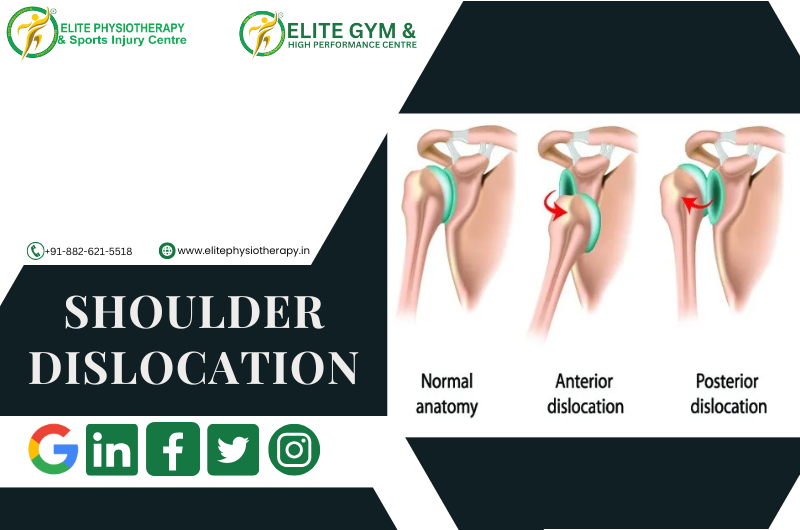
When the head of the humerus is violently separated from the scapula’s glenoid cavity, a shoulder dislocation takes place. Joint stability is compromised by this injury, which calls for quick and efficient treatment.
Causes of Shoulder Dislocation
- Trauma: Includes direct hits to the shoulder, falls, and motor vehicle accidents.
- Sports Injuries: Contact or high-impact sports, such as rugby, football, and wrestling.
- Repetitive strain: Caused by overhead tasks that gradually weaken shoulder tissues.
Due to its wide range of motion, the shoulder is prone to dislocation. The most frequent kind, anterior dislocations, are caused by an external force acting on an arm that has been abducted, stretched, and externally rotated. Although less frequent, posterior dislocations can happen as a result of internal rotation and arm adduction brought on by seizures or electric shocks.
Clinical Features
- Intense pain: Sudden, severe shoulder pain.
- Deformity: A noticeable change in the shape of the shoulders.
- Limited Mobility: Inability to move the arm without experiencing severe pain.
- Swelling and Bruising: Around the shoulder joint.
- Tingling or numbness: These symptoms could be signs of nerve involvement.
Diagnostic Approach at Elite Physiotherapy
Physical and Functional Assessment
Our clinicians conduct a thorough evaluation, including:
- Observation: Checking for muscle atrophy, edema, and deformity.
- Palpation: Recognizing soreness and unusual posture.
- Range of Motion Tests: Evaluating active and passive movements.
Special Physiotherapy Tests
Utilizing established orthopedic assessment techniques, we perform:
- Apprehension Test: By monitoring the patient’s response during external rotation and abduction, the Apprehension Test can identify anterior instability.
- Relocation Test: If symptoms improve when posterior pressure is applied, the relocation test confirms instability.
- Sulcus Sign: Identifies inferior instability by noticing a depression below the acromion when downward traction is given.
Imaging
While our primary focus is on physical assessment, we may recommend imaging studies like X-rays or MRIs to rule out fractures or soft tissue injuries if necessary.
Advanced Physiotherapy Management at Elite Physiotherapy
Our center offers a comprehensive, non-phase-wise rehabilitation program tailored to individual needs.
Pain Management
- Cryotherapy: Using cold packs to relieve pain and inflammation is known as cryotherapy.
- High-Intensity Class 4 Laser Therapy: Penetrating deeply into the tissue promotes tissue healing and lessens discomfort.
Restoring Mobility and Strength
Manual therapy:
- Joint mobilizations to improve mobility.
- Soft tissue techniques to alleviate muscle tightness and pain.
Therapeutic Exercises:
- Range of Motion (ROM): Mild motions to regain flexibility.
- Strengthening exercises: To improve joint stability, focus on the rotator cuff and scapular stabilizers.
- Proprioceptive Training: Enhancing neuromuscular control and joint position sensing through proprioceptive training.
Advanced Modalities
- Shock Wave Therapy: Beneficial for calcific tendinopathy and persistent shoulder discomfort.
- Capacitive and Resistive Electric Transfer (CRET) Therapy: Enhances tissue regeneration and reduces pain.
- The Super Inductive System (SIS) stimulates muscles and aids in healing by using strong electromagnetic fields.
- Hydrotherapy: Water-based exercises to improve mobility without stressing the joint.
Functional Rehabilitation:
It is the process of simulating everyday tasks to guarantee a safe transition back to regular functioning.
We focus on restoring functional independence through:
- Neuromuscular Re-education: Improving muscle control and coordination.
- Postural Training: Adjusting body alignment to avoid further injuries.
- Activity-Specific Training: Getting patients ready to resume sports or daily activities.
Why Choose Elite Physiotherapy & Sports Injury Centre?
- Expert Team: Skilled physiotherapists with a focus on musculoskeletal and Sports injuries.
- State-of-the-Art Facilities: Outfitted with cutting-edge techniques for the best possible care.
- Personalized Care: Customized treatment regimens to achieve certain objectives.
- Holistic Approach: Combining manual therapy, exercise, and cutting-edge technologies provides a holistic approach.
Conclusion
Quick and effective management of shoulder dislocations is essential to restore function and prevent recurrence. To guarantee the best possible recovery, we at Elite Physiotherapy & Sports Injury Centre provide thorough, evidence-based physiotherapy treatments using cutting-edge modalities. Our individualized approach aims to restore function, strength, and mobility so that patients can confidently resume their everyday activities and sports.