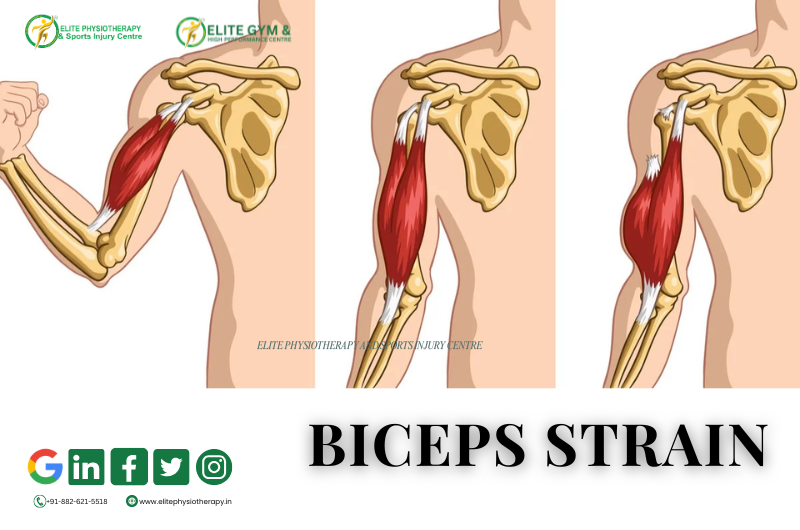
What is a Biceps Strain?
A biceps strain occurs when the biceps brachii muscle or its tendon is torn or overstretched. Usually, a high load or an abrupt force during arm movement causes it. The people most at risk are athletes, weightlifters, and those who lift objects repeatedly.
We frequently see biceps strains in athletes who participate in weightlifting, wrestling, boxing, and racket sports at Elite Physiotherapy and Sports Injury Centre. Early physiotherapy intervention ensures quicker recovery and prevents long-term muscle weakening.
Causes of Biceps Strain
Typically, biceps tension is caused by:
- Unexpected eccentric loading when throwing or lifting.
- Excessive usage of the arm repeatedly when performing overhead motions.
- Direct injury to the upper arm or impact.
- Improper lifting technique or improper warm-up.
- Loss of control and stability due to muscle exhaustion.
These elements may result in microtears in the tendon or muscle fibers, which would induce discomfort and inflammation.
Classification of Biceps Strain
The degree of muscle fiber damage determines the classification of biceps strains:
- Grade 1 (Mild): No strength loss, little discomfort, and minimal fiber ripping.
- Grade 2 (Moderate): Partial tear accompanied by discomfort, edema, and diminished strength.
- Grade 3 (Severe): Total rupture of a muscle or tendon, frequently accompanied by a protrusion or “Popeye deformity.”
A thorough clinical evaluation at Elite Physiotherapy aids in determining the precise grade and creating a customized rehabilitation strategy.
Clinical Features and Symptoms
Typical signs and symptoms include:
- The front of the arm hurts sharply.
- Soreness and swelling above the biceps.
- Discolouration or bruises.
- Weakness occurs when the forearms are supinated or the elbows are bent.
- Tightness in the muscles and trouble lifting things.
- Obvious deformity brought on by tendon retraction in extreme situations.
- When the biceps muscle is actively contracted or stretched, pain increases.
Diagnostic Methods and Examination
A thorough patient history and physical examination are the first steps in a clinical diagnosis. To ascertain the injury grade, the physiotherapists at Elite Physiotherapy employ a mix of muscle testing, palpation, and examination.
Special Physiotherapy Tests
- Biceps Squeeze Test – Helps detect complete rupture of the distal biceps tendon.
- Speed’s Test: Determines whether there is tendinous involvement by measuring pain over the bicipital groove.
- Yergason’s Test: Identifies instability in the bicipital groove or pathology in the long head of the biceps tendon.
These tests aid in distinguishing between tendinous damage and muscle belly strain.
Investigations
- Ultrasound: To detect muscle fiber tears and hematomas.
- MRI: For severe or chronic cases to assess tendon retraction or complete rupture.
Physiotherapy Management at Elite Physiotherapy and Sports Injury Centre
At Elite Physiotherapy, treatment focuses on pain reduction, restoring strength, and preventing recurrence. Physiotherapists tailor each plan according to the athlete’s sport demands, injury grade, and recovery goals.
Acute Phase (First 3–5 Days):
- The aim is to reduce pain, inflammation, and swelling through rest, ice, compression, and elevation (RICE) principles. Physiotherapists use advanced modalities such as High-Intensity Laser Therapy (HILT) to accelerate tissue repair and reduce inflammation, while the Super Inductive System (SIS) aids in pain modulation and early muscle activation. Gentle kinesio taping supports the injured muscle and prevents further strain.
Subacute Phase (After 5–10 Days):
- The focus shifts to restoring flexibility and preventing stiffness. Pain-free active and assisted range of motion exercises are introduced for the elbow and shoulder. Shock Wave Therapy enhances collagen production and promotes tendon healing, whereas Cupping Therapy improves local blood flow and reduces muscle tightness. Physiotherapists apply Dry Needling to deactivate trigger points and reduce muscle tension. Gradual isometric strengthening begins to re-engage the biceps muscle safely.
Strengthening and Functional Phase (After 2–3 Weeks):
- Once pain subsides, the goal is to rebuild strength and endurance through progressive resistance training, emphasizing eccentric biceps loading. Physiotherapists add functional and sport-specific exercises along with shoulder stabilizer strengthening to improve kinetic chain coordination. The Super Inductive System (SIS) continues to support deep tissue healing and enhance neuromuscular re-education.
Return-to-Sport Phase:
- The final stage prepares the athlete for competition or full activity. Sport-specific drills, plyometric exercises, and movement retraining are implemented to restore full functional capacity. Physiotherapists conduct postural correction and strength balance assessments to prevent recurrence. Before clearance, the patient must demonstrate full range of motion, pain-free strength, and proper biomechanics.
- Advanced Modalities Used at Elite Physiotherapy
This combination ensures quicker recovery, reduced pain, and improved performance — helping athletes return to training stronger than before.
Conclusion
If left untreated, a biceps strain can impair arm function and athletic performance. Our state-of-the-art rehabilitation method at Elite Physiotherapy and Sports Injury Centre blends manual treatment with innovative techniques, including Shock Wave, SIS, HILT, Dry Needling, and Cupping.
Athletes who receive individualized care heal more quickly, regain their confidence, and safely resume their best performance.