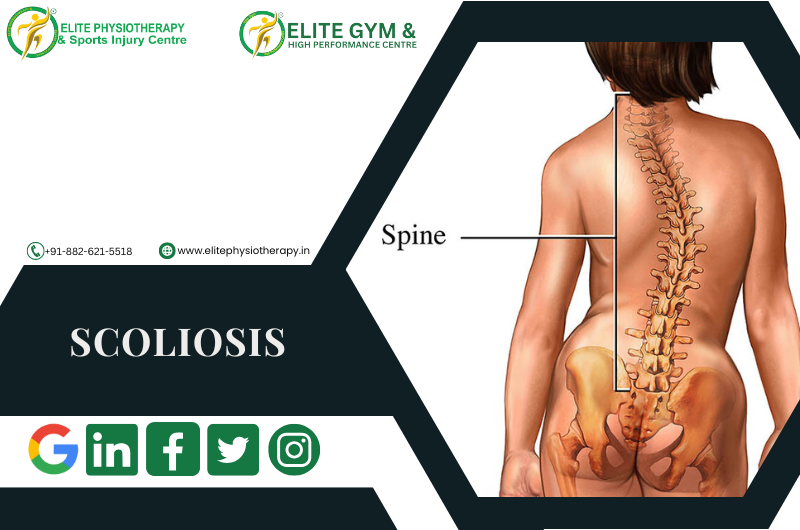
What Is Scoliosis?
Scoliosis is a three-dimensional spinal deformity characterized by both vertebral rotation (in the axial plane) and lateral curvature of the spine (in the coronal plane). One side of the back may protrude more than the other while bending forward, and the spine may resemble an “S” or “C” when viewed from behind. Scoliosis is typically defined as a curvature of 10 degrees or more, as determined by the Cobb technique.
It is a complicated three-plane problem since sagittal curvatures (kyphosis, lordosis) frequently change beyond the coronal deformity.
In the context of sports injuries and specialist physiotherapy, early identification, thorough evaluation, and customized rehabilitation can aid in managing progression, reducing symptoms, and enhancing function.
Causes & Contributing Factors
Scoliosis arises from multiple possible causes; many cases have an unknown origin. Here are key categories:
1. Idiopathic scoliosis
- The most prevalent kind, particularly in teenagers (ages 10–18).
- Subtypes include infantile, juvenile, and adolescent idiopathic.
2. Congenital scoliosis
- As a result of birth-related vertebral abnormalities (hemivertebra, vertebral fusion).
3. Neuromuscular scoliosis
- Linked to neuromuscular disorders, such as spinal cord damage, cerebral palsy, and muscular dystrophy.
4. Degenerative (de novo) scoliosis
- Occurs in adults due to osteoporosis, facet arthropathy, and disc degeneration.
5. Functional (postural, non-structural) scoliosis
- Adaptable curvature without rotation of the vertebrae.
- When the underlying cause (muscle spasm, leg-length disparity) is addressed, it goes away.
Types & Classification
To understand and manage scoliosis, clinicians use classifications based on various dimensions:
By Etiology
Idiopathic, congenital, neuromuscular, degenerative, functional (as above)
By Age of Presentation
- Infantile (< 3 years)
- Juvenile (4–10 years)
- Adolescent (> 10 years)
Curve Magnitude (Cobb Angle)
- Mild: < 20°
- Moderate: 20°–40° (or 25°–50° in some sources)
- Severe: > 45°–50°
By Curve Location / Pattern
- Thoracic curve
- Thoracolumbar curve
- Lumbar curve
- Double / S-shaped curves (two curves)
- Single or compensatory curves
By Structural Rigidity
- Structural scoliosis: Fixed curve with spinal rotation and structural alterations.
- Non-structural / functional scoliosis: Flexible curvature, no rotation, and reversible by specific motions.
Clinical Features, Signs & Symptoms
While not everyone with scoliosis exhibits symptoms, common clinical characteristics include:
- Asymmetry in the trunk that is visible (uneven shoulder heights, scapular prominence)
- Prominence or hump in the ribs when leaning forward
- Leg-length disparity, pelvic tilt, or uneven waistline
- Particularly in people with degenerative changes, back pain
- Stiffness or exhaustion in the paraspinal muscles
- limited range of motion in the spine
- Reduced chest expansion and respiratory impairment in severe curvature
Upon physical examination, one could note:
- Unbalanced paraspinal muscle mass
- prominent concave side rib hump
- Trunk shift over the pelvis
- Variation in the alignment of the spinous process
- Variations in posture when walking and standing
When asymmetry is detected, young patients frequently show up through school screening (such as Adam’s forward-bend test).
Physical Tests & Assessment Techniques
Assess paraspinal muscle tightness or tenderness.
Special Orthopedic Tests
1. Adam’s Test of the Forward Bend
Examiners look for rib protrusion or asymmetry from behind.
2. Inclinometer/Scoliometer
When bending forward, the angle of trunk rotation, or ATR, is measured.
helps measure the prominence of the rib hump.
3. Landmarks of the spine and palpation
To find rotation or lateral deviation, feel for spinous processes.
4. Testing for Range of Motion (ROM)
trunk rotation, flexion/extension, and lateral flexion
Compare the flexibility from side to side.
5. Measurement of Leg Length
To eliminate the possibility that a leg-length disparity is causing a functional curve
Assess the curve’s flexibility using the side-bending test to see if it bends correctly. Torsional stress tests and the difference between the ribs and vertebrae. Provocative testing for disc, facet, and nerve root involvement; segmental vertebral mobility tests (passive intervertebral motion)
Physiotherapy Management Strategies
At Elite Physiotherapy & Sports Injury Centre, we emphasize evidence-based, patient-centred interventions. Our goal is to slow or halt curve progression, reduce pain, restore alignment and mobility, and enhance function.
1. Physiotherapeutic Scoliosis-Specific Exercises (PSSE / 3D Correction)
These specific remedial workouts are made to fit the curvature pattern of each patient. Among the principles are:
- Self-correction in three dimensions: Active correction in the transverse, sagittal, and coronal planes
- Stabilization of the posture correction
- Breathing exercises to de-rotate the rib cage and extend the concave side
- Integration with ADLs (training for habitual posture)
- Balance, core activation, and sensorimotor training
2. Manual Therapy & Mobilization
- Gentle spinal mobilization of restricted segments
- Myofascial release and soft tissue mobilization of tense muscles on the convex side
- Increasing thoracic mobility using rib mobilization
- Elongated muscle strengthening and shortened muscle stretching
3. Core Stabilization & Motor Control Training
- Activation of deep trunk muscles (transverse abdominis, multifidus)
- During movement, functional trunk control
- Training for balance and proprioception
4. Electro-physical Modalities
Through pain relief, soft tissue modulation, and improved muscle function, these modalities can be used in conjunction with active and manual approaches. Each modality may be integrated as follows:
- Shock Wave Therapy
- Super inductive system
- High-Intensity Laser Therapy
- Cupping and Dry Needling
5. Bracing / Orthosis (in collaboration with orthopedics)
- When indicated (moderate curves in growing patients), physiotherapy works alongside bracing:
- Teach patients how to perform corrective exercises within the brace
- Postural coaching with brace off
- Strengthening to manage brace-induced weakness
Why Patients Should Choose Elite Physiotherapy & Sports Injury Centre
At Elite, we bring together:
- proficiency in spinal and musculoskeletal care
- Personalized procedures for scoliosis
- Availability of auxiliary cutting-edge modalities such as high-intensity laser, shock wave, and Super Inductive System
- Prioritize functional rehabilitation so you can resume your daily activities or sports.
- Thorough monitoring, follow-up, and high-quality results
Conclusion
Being a complicated, three-dimensional abnormality, scoliosis necessitates meticulous evaluation, specialized treatment, and regular monitoring. At Elite Physiotherapy & Sports Injury Centre, we provide patients with a comprehensive, evidence-based treatment plan that includes everything from functional reintegration and long-term monitoring to precise orthopedic physical assessment, curve-specific corrective techniques, supportive modalities like shock wave, Super Inductive system, high-intensity laser, and selective dry needling or cupping.
We seek to control curve progression, reduce discomfort, improve mobility, and assist you in leading an active, satisfying life by emphasizing individualized rehabilitation.